Abstract _ Full Text (HTML) _ Full Text (PDF)
Case Report
Cancer Research Frontiers. 2017; 3(1): 51-55. doi: 10.17980/2017.51
Primary B-cell lymphoma of the pelvis bone in a young patient: Imaging features of a rare case.
Nghi C. Nguyen1*, Mujahid Khan1, Muhammad Shah1
1Department of Radiology, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania.
*Corresponding author: Nghi C. Nguyen, MD, PhD, Assistant Professor of Radiology, University of Pittsburgh. UPMC Presbyterian, 200 Lothrop Street (at Meyran Ave), East Wing, 2nd Floor, Suite 200, Pittsburgh, PA 15213. Phone: 412-647-0104; E-mail:
Citation: Nghi Nguyen, et al. Primary B-cell lymphoma of the pelvic bone in a young patient: Imaging features of a rare case. Cancer Research Frontiers. 2017; 3(1): 51-55. doi: 10.17980/2017.51
Copyright: @ 2017 Nghi Nguyen, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing Interests: The authors declare no competing financial interests.
Received Feb 24, 2017; Revised Apr 17, 2017; Accepted Apr 24, 2017. Published May 9, 2017.
Abstract
Bone scan of an 18-year-old male who initially presented with chronic left knee pain showed increased radiotracer uptake in the left knee indicative of osteoarthritis. For the incidental finding of diffusely intense uptake involving the left hemipelvis, Paget’s disease was favored over osteosarcoma and Ewing’s sarcoma. CT scan without IV contrast showed cortical and trabecular thickening of the hemipelvis. However, it was not until the MRI study that showed findings inconsistent with Paget’s disease and suspected primary bone lymphoma because of the extensive T1 signal loss due to bone marrow replacement with contrast enhancing soft tissue in the absence of cortical bone destruction, with histopathology revealing extranodal diffuse large B-cell lymphoma. We present a rare case of Non-Hodgkin’s lymphoma occurred in a young patient and illustrate the diagnostic difficulty of primary bone lymphoma as well as emphasize the importance of multi-modality correlation for the differential diagnosis of Paget’s disease vs. primary bone lymphoma.
Keywords: Primary bone lymphoma; B-cell lymphoma; radionuclide bone scan; computed tomography; magnetic resonance imaging
Introduction
Primary bone lymphoma is encountered in approximately 3-7% of primary bone tumors. The majority of the cases represent limited disease with an age predilection of 20-50 years (1-3). Rare cases may be seen in children with a mean age of 12 years (4). Primary bone lymphoma may be difficult to diagnose unless there is a high level of suspicion. Multi-modality imaging may be warranted for proper diagnosis.
Case report
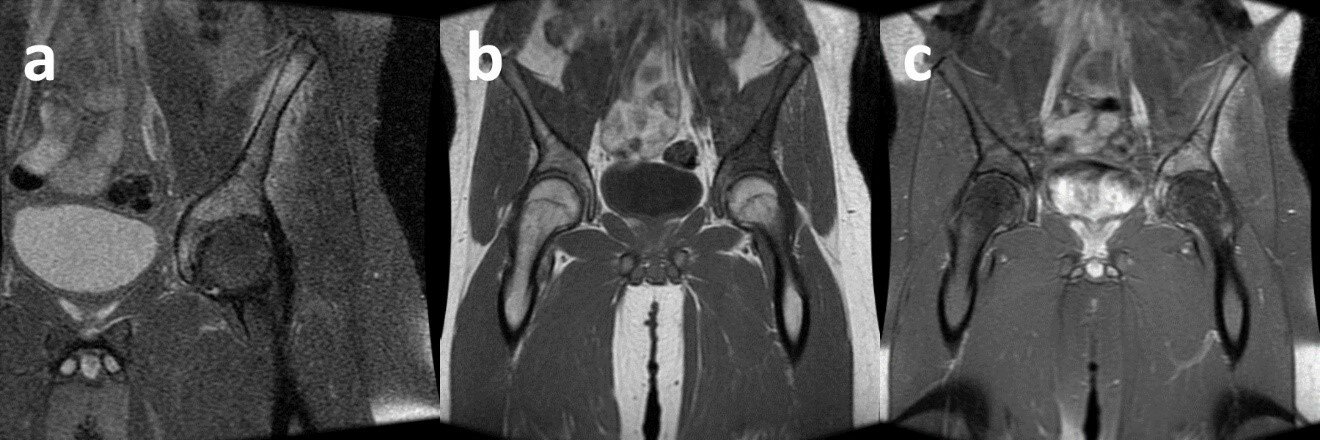
An 18-year-old male presented with intermittent left knee pain. His knee x-ray was unremarkable, and because he was very active working out in the gym and playing sports, he felt that he had an injury secondary to his sports activities. He participated in physical therapy for one month, but his pain did not subside. A whole-body bone scan with Tc-99m methyl diphosphonate was then performed six months after his initial presentation, which showed a small focus of mild radiotracer uptake in the left femoral-patellar joint indicative of osteoarthritis (Figure 1). For the incidental finding of diffusely intense tracer uptake involving the left hemipelvis, Paget’s disease was favored, although osteosarcoma and Ewing’s sarcoma were also considered. Upon further questioning, the patient endorsed the more recent development of pain in the left groin and thigh. He had B symptoms with night sweats without fever and 20 lbs weight loss within the last 6 months. Subsequent computed tomography (CT) scan without intravenous contrast showed diffuse cortical and trabecular thickening of the hemipelvis, but the typical trabecular coarsening seen in Paget’s disease was not present (Figure 2). Further evaluation with magnetic resonance imaging (MRI) scan with intravenous contrast media showed extensive T1 bone marrow signal loss throughout the left ilium extending onto the left ischium and acetabulum with associated gadolinium contrast enhancement, which indicated bone marrow replacement by a malignant lymphoproliferative process. The cortex was intact, and there was a circumferential layer of abnormal enhancing soft tissue surrounding the cortex (Figure 3). MRI findings raised the suspicion for primary bone lymphoma which prompted a core biopsy revealing diffuse large B-cell lymphoma, germinal center subtype, which appeared to involve the bone with prominent intra-trabecular fibrosis and focal areas of necrosis. The tumor was positive for CD20, Ki-67 (>50%) and negative for BCL2, BCL6, and c-MYC. CT abdomen and pelvis demonstrated mild splenomegaly without focal lesions and no evidence of abdominal and pelvic lymphadenopathy; no FDG PET scanning was however obtained prior to therapy. The patient was found to have stage IVE disease according to the International Extranodal Lymphoma Study Group (IELSG), with extensive bone marrow lesions involving the left hemipelvis (3). His Revised International Prognostic Index (R-IPI) score was 2, with elevated LDH 209 U/L (upper normal < 171), ECOG grade 2. C-reactive protein was 4.86. Given the negative FISH markers and molecular studies that did not reveal a double or triple hit lymphoma, the treatment option for his stage IVE disease was largely limited to chemotherapy. He achieved complete remission after four cycles of R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone) and has been free from disease for 14 months. No FDG PET scanning for initial staging was obtained, but an FDG PET scan after 4 cycles of chemotherapy performed at an outside facility showed no FDG avid lesions to suspect residual or recurrent disease; images were not available for review. Follow-up evaluations included LDH, CBC and differential blood count as well as CT scans, all of which were unremarkable.
Figure 1. An 18-year-old male underwent bone scan for a six-month history of left knee pain. Anterior and posterior whole-body (a, b), anterior and posterior pelvis (c, d) bone scan images were obtained three hours after the IV administration of 27.5 mCi of Tc-99m methyl diphosphonate.
Figure 2. CT scan following bone scan in this patient shows diffuse cortical and trabecular thickening of the hemipelvis supporting the diagnosis of Paget’s disease.
Discussion
Incidental finding of diffusely increased tracer uptake involving the left hemipelvis is commonly seen in Paget’s disease, considering that the pelvis represents one of the most frequent sites of involvement besides the spine (30-75% of cases) (5). The radionuclide uptake at bone scanning is typically increased in all three phases of Paget’s disease (osteolytic, mixed, and osteoblastic), and the diffuse uptake of the hemipelvis is commonly seen in Paget’s disease. Although bone scan is sensitive for the detection of hypervascularity and osteoblastic activity in Paget’s disease, it lacks specificity which may lead to occasional pitfalls as shown in this case of extranodal diffuse large B-cell lymphoma. In addition to bone scanning, x-ray or CT is typically acquired for further correlation, and radiographic findings of Paget’s disease are largely identical to CT findings (5). An x-ray was not performed in this case. The CT scan did not show significant trabecular coarsening typically seen in Paget’s disease. Instead, there was diffuse cortical and trabecular thickening of the left hemipelvis which might indicate primary bone lymphoma, although CT findings of primary bone lymphoma are often nonspecific and a variety of neoplasms may be considered in the differential diagnosis (6).
Primary lymphoma of bone as a rare type of lymphoma arising from the bone occurs in approximately 5% of extranodal non-Hodgin’s lymphoma. The vast majority of cases is non-Hodgkin’s lymphoma, and less than 5% is Hodgkin’s lymphoma (1, 7). Monostotic or polyostotic disease involving the long bones are typical, with the femur being the most common site (29%), but other common sites include the pelvis and spine (2-4, 8). Compared to the rather nonspecific CT findings of diffuse cortical and trabecular thickening, the MRI provides significant added value because of its high soft tissue contrast and high sensitivity for bone marrow abnormalities (9, 10). The extensive bone marrow replacement with contrast-enhancing soft tissue combined with the intact bone cortex on MRI suggest primary bone lymphoma, although the differential diagnosis also includes Ewing’s sarcoma and osteosarcoma considering the patient’s age (7). Paget’s disease is unlikely because of the fat signal loss on pre-contrast T1, which is typically preserved in Paget’s disease (5, 10). Sarcomatous degeneration of Paget’s disease is unlikely in this patient because of his age and the rare occurrence (approximately 1%) in older patients with longstanding Paget’s disease (5). At MRI, primary bone lymphoma is commonly hypo-intense on T1-weighted images, but the appearance of T2-weighted images varies from hyperintense as seen in this case, to isointense and hypointense (6, 9, 10). Although some of the decreased signal intensity (hypointense) on T2-weighted images may be attributed to the fibrous content within the tumor, the etiology of the variable T2 signal intensities is not well characterized (9). Tumor spread along the long axis of the bone without frank cortical destruction is common in primary bone lymphoma. Other imaging features include periosteal reaction and soft tissue extension as well as pathologic fracture and cord compression (2, 4, 11). This case report illustrates the diagnostic difficulty of primary bone lymphoma and emphasizes the importance of multi-modality correlation for the differential diagnosis of Paget’s disease vs. primary bone lymphoma.
Figure 3. Coronal MRI imaging of the pelvis – pre-contrast T2-weighted with fat saturation (a); pre-contrast T1-weighted image without fat saturation (b); post-contrast (20 ml MultiHance) T1-weighted with fat saturation (c). The iliac bone demonstrates diffuse hyperintensity on T2 and hypodensity on T1 with subsequent contrast enhancement on T1. The bone cortex appears intact although there is a layer of contrast enhancement in the periosteal soft tissue. MRI findings were suspicious for primary bone lymphoma.
Abbreviations:
Bcl-2, B-cell lymphoma 2
Bcl-6, B-cell lymphoma 6
CBC, complete blood count
CT, computed tomography
LDH, lactate dehydrogenase
MRI, magnetic resonance imaging
References
- Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphomas. Cancer. 1972 Jan;29(1):252-60.
- Stein ME, Kuten A, Gez E, Rosenblatt KE, Drumea K, Ben-Shachar M, et al. Primary lymphoma of bone–a retrospective study. Experience at the Northern Israel Oncology Center (1979-2000). Oncology. 2003;64(4):322-7. DOI: 10.1159/000070288.
- Messina C, Christie D, Zucca E, Gospodarowicz M, Ferreri AJ. Primary and secondary bone lymphomas. Cancer Treatment Reviews. 2015 Mar;41(3):235-46. DOI: 10.1016/j.ctrv.2015.02.001.
- Glotzbecker MP, Kersun LS, Choi JK, Wills BP, Schaffer AA, Dormans JP. Primary non-Hodgkin’s lymphoma of bone in children. J Bone Joint Surg Am. 2006 Mar;88(3):583-94. DOI: 10.2106/JBJS.D.01967.
- Smith SE, Murphey MD, Motamedi K, Mulligan ME, Resnik CS, Gannon FH. From the archives of the AFIP. Radiologic spectrum of Paget disease of bone and its complications with pathologic correlation. Radiographics. 2002 Sep-Oct;22(5):1191-216. DOI: 10.1148/radiographics.22.5.g02se281191.
- Girish G, Finlay K, Fessell D, Pai D, Dong Q, Jamadar D. Imaging review of skeletal tumors of the pelvis malignant tumors and tumor mimics. ScientificWorldJournal. 2012;2012:240281. DOI: 10.1100/2012/240281.
- Mulligan ME, McRae GA, Murphey MD. Imaging features of primary lymphoma of bone. AJR Am J Roentgenol. 1999 Dec;173(6):1691-7. DOI: 10.2214/ajr.173.6.10584821.
- Ramadan KM, Shenkier T, Sehn LH, Gascoyne RD, Connors JM. A clinicopathological retrospective study of 131 patients with primary bone lymphoma: a population-based study of successively treated cohorts from the British Columbia Cancer Agency. Ann Oncol. 2007 Jan;18(1):129-35. DOI: 10.1093/annonc/mdl329.
- Stiglbauer R, Augustin I, Kramer J, Schurawitzki H, Imhof H, Radaszkiewicz T. MRI in the diagnosis of primary lymphoma of bone: correlation with histopathology. J Comput Assist Tomogr. 1992 Mar-Apr;16(2):248-53.
- White LM, Schweitzer ME, Khalili K, Howarth DJ, Wunder JS, Bell RS. MR imaging of primary lymphoma of bone: variability of T2-weighted signal intensity. AJR Am J Roentgenol. 1998 May;170(5):1243-7.
- Girish G, Finlay K, Morag Y, Brandon C, Jacobson J, Jamadar D. Imaging review of skeletal tumors of the pelvis–part I: benign tumors of the pelvis. ScientificWorldJournal. 2012;2012:290930. DOI: 10.1100/2012/290930.